Pre-fuzzy front end alignment of multiple stakeholders in healthcare service innovation: Unpacking complexity through service and systems oriented design in Strategy Sandboxes
Rygh, Karianne, Morrison, Andrew, Støren Berg, Marianne and Romm, Jonathan (2018) Pre-fuzzy front end alignment of multiple stakeholders in healthcare service innovation: Unpacking complexity through service and systems oriented design in Strategy Sandboxes. In: Proceedings of RSD7, Relating Systems Thinking and Design 7, 23-26 Oct 2018, Turin, Italy.
![Rygh_MM_2018.jpg [thumbnail of Rygh_MM_2018.jpg]](https://openresearch.ocadu.ca/2733/1.hassmallThumbnailVersion/Rygh_MM_2018.jpg) 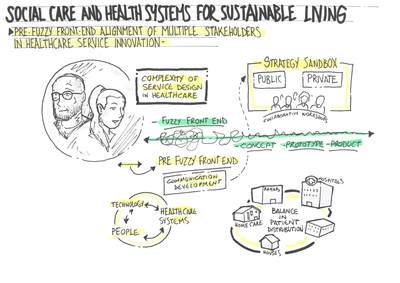 Preview |
Image
Rygh_MM_2018.jpg Download (333kB) | Preview |
Abstract
Introduction
Contemporary health systems are deeply complex, organisationally and temporally. Recently, focus has increasingly been given to patient experiences and needs (LaVela & Gallan, 2014) and to developing services that accommodate a diversity of needs within formal institutions and their extensions into society. With patient-centred recovery and well-being as a focus, the challenge arises as to how innovative and sustainable services can be developed in contexts of such systems. While Service Design (SD) has emerged as a domain of design-based inquiry and professional practice, early studies have often centred on commercial partners, service delivery, customer experience and satisfaction views. However, such approaches ought to be coupled with Systemic Design efforts, due to the socio-technological complexity and interlinked nature of healthcare service development and change management (Jones, 2013). This is crucial in the front-end of related design.
In the Nordic countries, the public healthcare sector is seeking to increase partnerships with private actors in order to reach policy goals and offer healthcare services to a wider demographic in a time of resource shortage. Ensuring a fruitful collaboration between public and private sectors becomes central as a matter of design and innovation. Such collaborations also amount to complex social systems, where actors need to understand patient journeys and medical procedures, co-create innovative solutions and distribute ownership, assignments and risks. Establishing collaborative partnerships between healthcare actors and private commercial actors can be challenging due to the deeply institutionalised ways of working and siloed expertise of the medical sector.
This calls for processes and tools that support communication and alignment of diverse actors’ views embedded in such complex social systems to be further developed and better understood systemically. This is especially crucial in the front end of related design, often referred to as the ‘fuzzy front end’. The authors have tackled these challenges facing innovative partnerships through the development and proposal of a Strategy Sandbox workshop pilot.
Developing a Strategy Sandbox for healthcare service innovation
Innovation processes are often divided in three areas: the fuzzy-front end (FFE), new product development (NPD) and commercialisation (Koen et al., 2002). The FFE determines what is to be developed on a conceptual level, but does not develop the details for a specific solution, hence the term ‘fuzzy’. In healthcare cross-sector collaborations, all actors need to gain an understanding of patient journeys and medical procedures early on, to be able to co-create innovative concepts and make a planning for the distribution of ownership, assignments and risks. This paper therefore proposes the introduction of a preliminary phase of the FFE, termed the ‘pre-fuzzy front end’ (PFFE), supporting an alignment of relationships between participating actors and the co-creation of a shared understanding of the object of development before entering the FFE.
Through defining the PFFE, the authors have questioned:How may service design support multiple actors (public and private) in aligning their expectations, needs and goals to co-envision new directions for patient-centric healthcare service innovation in the pre-fuzzy front end of a development process?
Rooted in qualitative inquiry and practice based research, the authors have made use of a blend of methods to approach this question: research by design, reflection on action and analysis of data such as sketches photographs and contextually designed facilitation tools that unpack the fuzzy front end site in wider reflexive and iterative innovation processes.
Understanding the complexity of service-system relations
The sandbox metaphor is borrowed from innovation processes and product R&D and is perceived as a conceptual workspace encouraging exploration, experimentation and interaction between diverse actors. It is informed by the Centre for Connected Care (C3) research investigating innovation labs (Carstensen & Bason, 2012) and co-design communication tools (Sanders & Stappers, 2008) that are used within the context of healthcare service design. The research draws parallels to design oriented innovation venues in health, e.g. the 100-days challenge of Nesta Health lab (UK), Experio lab (Sweden) and Mindlab (Denmark).
One of the features of complex systems is layering, meaning that different phenomena and unpredictable qualities can appear at different levels of aggregation and spatial scale (Liljenstrom & Svedin, 2005). The Strategy Sandbox has therefore set out to unpack the complexity of healthcare service development on three levels: Macro (mapping stakeholders needs), micro (mapping user needs and experiences) and meso (co-envisioning and co-developing possibility areas). Sandboxes have also been described as having four key features: connectors, framing, space and speed (Clarke, 2017). The workshops explored early phase formation of innovative partnerships within the C3 stroke project. With 47 participants in total, the concept has been run as an innovation partnership and public procurement between public sector actors and commercial vendors to innovate products and services to address unmet needs.
Workshop 1
Working on a macro level, the first workshop aimed at aligning the participating actors by creating a shared overview of their needs and perspectives, allowing them to express their opinions and views. Tailored communication tools mediated discussions between workshop participants, facilitating the sharing of perspectives on the service situation and proposals of possible public private partnerships. (Figure 1).
Actor needs were filtered via criteria derived from medical health professionals, designers and participants where a visual relational mapping clarified available resources in the actor network. By using physical tools, concepts were re-evaluated and adapted leading to concept shifts (Buur, 2012) where a proposal was presented regarding what a med-tech company might offer in developing innovative purchases following defined needs. This, we see as a systems oriented design mode of exploring service networks.
Workshop 2
On a micro level, the second workshop facilitated a detailed mapping of users’ needs and experiences and an exploration of different public-private partnerships. Here, we sought to unpack systemic complexity in two ways: 1) mapping patient needs and experiences, and 2) exploring partnership possibilities for technology, users and health service professionals. The workshop made apparent patient views through their participative engagement in patient journey experience mapping, specifically in transitional parts of the service trajectory.
Between workshops, project team meetings were held to reflect on and analyse the previously generated data, leading to plans and strategies for the next workshop. Ten possible areas of development were identified and used as a basis for workshop number three.
Workshop 3
The third workshop of the Strategy Sandbox was dedicated to co-assessment and co-development of the identified possibility areas on a meso level. Evaluations of previous mappings and explorations to develop ten possibility areas for new systemically situated service development, were evaluated and revised to: 1) strengthen patient cognitive assessment, 2) secure further and consistent treatment practices, 3) empower the patient, family and carer givers, and 4) implement distance monitoring and digital touchpoints. To facilitate the evaluation and selection of focus areas for the wider project, a holistically oriented health technology co-assessment tool was developed by the authors (Figure 2).
Future pathways
Through utilising a service systems design process and taking a ‘pre-fuzzy front end’ approach to strategy sandboxes, the stroke project managed to leverage proposals of strategies for matching the aims of technology partners with the service directions of the public healthcare actors. The workshop process facilitated an alignment of expectations and goals amongst participating actors, an identification of needs both for participating actors and end users, and co-envisioned directions for service innovation within the topic of stroke.
Service systems relations are layered and entangled and take time to be understood by a wide network of diverse actors. Our inquiry this far indicates that in order to accommodate the time needed to develop an understanding of the complex relations involved in healthcare collaborations, there is a need for a pre-fuzzy front end alignment phase within service innovation processes. Furthermore, to support the development of more sustainable and accessible healthcare services, this pre-fuzzy front end phase can greatly benefit from more systems oriented design approaches being incorporated into strategic workshop facilitation design.
| Item Type: | Conference/Workshop Item (Lecture) |
|---|---|
| Uncontrolled Keywords: | Healthcare, Service-system design, Workshop facilitation, Strategy sandbox, Co-design, Innovation, Service design |
| Related URLs: | |
| Date Deposited: | 10 Jul 2019 21:39 |
| Last Modified: | 16 Aug 2021 16:28 |
| URI: | https://openresearch.ocadu.ca/id/eprint/2733 |
Actions (login required)
 |
Edit View |
 Lists
Lists Lists
Lists